Abstract
The objectives of this study were to investigate (1) gender and race differences in mental health and psychological well-being among older adults during the COVID-19 pandemic and (2) whether there were significant interaction effects between gender and race. This study used the National Health and Aging Trends Study (NHATS) and COVID-19 public use data files. It focused on mental health and psychological well-being, including loneliness, no time to yourself, poor sleep quality, anxiety, depression, and post-traumatic stress disorder (PTSD). The sample consisted of 2465 older adults, and multivariate logistic and linear regression models were adopted for the analysis. The results show that approximately two out of five older people (43%) experienced poor sleep, followed by loneliness (35%), anxiety (30%), depression (23%), and no time to themselves (11%). The average PTSD score was 11. Mental health and psychological well-being varied by gender and race. There were significant interaction effects on anxiety and depression between females and Black older adults. Black females reported lower levels of anxiety and depressive symptoms than Black males, although the differences were not statistically significant. Black older adults were more likely to experience PTSD but less likely to feel lonely and have poorer sleep than their White counterparts. Female older adults reported poorer mental health and psychological well-being than males, except for Black females. Black females had the lowest levels of anxiety, depression, loneliness, and highest quality of sleep among all females of different ethnic and racial origins.
Similar content being viewed by others
1 Introduction
Since December 2019, the novel coronavirus disease (COVID-19) has impacted various aspects of older people’s lives and their families. Advanced age-associated chronic conditions and frailty greatly increase older adults’ risk of symptom severity and mortality (Azar et al. 2020; Xu and Arling 2023). As a potent stressor and traumatic event, COVID-19 has significantly increased older adults’ vulnerability to anxiety, depression, loneliness, poor sleep quality, and post-traumatic stress symptoms (PTSD) (Carr 2021; Lalani et al. 2023). A combination of factors has contributed to the negative impact on older adults’ mental health and well-being such as the extensive media coverage, the accumulating cases and disproportionately high mortality in older adults, fear of exposure, disruptions in their healthcare, uncertainty of the future, and lack of social support (Alobuia et al. 2020; Webb and Chen 2022; Xu and Arling 2023; Lalani et al. 2023). However, it is interesting to note that these differences varied differently among older people of different gender, race, and ethnicity (Boserup et al. 2020; Galasso et al. 2020). Therefore, there is a need to adopt a gender and racial lens to examine the effects of the pandemic on older adults and its impacts on their mental health and well-being.
Multiple studies have shown the importance of gender differences on the impact of COVID-19. Men with COVID-19 in comparison to women were more likely to have worse outcomes and death, independent of age (Jin et al. 2020; Ya’qoub et al. 2021). Studies also found that there were gender differences in pandemic perception and action (Galasso et al. 2020; Ferrín 2022). A study of 21,649 participants in eight Organization for Economic Co-operation and Development countries found that women were more likely to perceive the pandemic as a serious health problem and were more likely to agree and comply with restraining public policy measures (Galasso et al. 2020). Meanwhile, studies on psychological response to the pandemic suggested that women experienced higher levels of anxiety, depression, and acute stress than men (García‐Fernández et al. 2021; Laufer and Shechory Bitton 2021). Therefore, in the context of the pandemic, it is necessary to further investigate the potential negative impact on older adults’ mental health and well-being, particularly on women.
Similarly, research has pointed out the differential impacts of COVID-19 on racial and ethnic groups. Racial and ethnic minorities have suffered disproportionately high rates of COVID-19 incidence, hospitalization, and mortality (Azar et al. 2020; Boserup et al. 2020; Garcia et al. 2021; Muñoz-Price et al. 2020; Price-Haywood et al. 2020). Racial and ethnic minorities also had lower levels of knowledge and attitudes (for example, concerns and stress about its negative impacts on their lives) related to COVID-19 but demonstrated better practices to reduce the risk of COVID-19 (Alobuia et al. 2020). Frail non-White older people were more likely to put off needed or planned care during the pandemic than their White counterparts (Xu and Arling 2023). Regarding mental health, Black, Hispanic, and Asian adults were more likely to experience anxiety and depression and had higher levels of unmet mental health care needs during the pandemic compared to White individuals (Thomeer et al. 2023). However, the racial and ethnic differences in mental health are not absolute. Goldmann et al. (2021) found reverse relationships. Despite the greater experience of COVID-19-related stressors, Black, Hispanic, and Asian adults had lower odds of anxiety and depression symptoms compared to their White counterparts (Goldmann et al. 2021). There is a need to further investigate racial and ethnic differences in mental health and well-being among the older population. Reducing health disparities among older adults is a major priority for policymakers and healthcare systems with the increasing aging population and related complexities of elderly care around the globe.
Several gaps were identified in previous studies that examined gender and racial differences in mental health and well-being. Most studies have an unrepresentative study population with relatively small sample sizes (Gamsızkan et al. 2021; Willey et al. 2022). Many studies include all adults rather than assigning them to specific adult age ranges or criteria (Zhao et al. 2020; Thomeer et al. 2023). Older adults are the most vulnerable population to COVID-19 and their experiences may be different from young and middle-aged adults. Research has tended to emphasize gender differences and race differences separately without considering the potential interactions between gender and race (Goldmann et al. 2021; Riehm et al. 2021; Willey et al. 2022). Moreover, a lot of studies focused only on depression and anxiety among older adults (Zhao et al. 2020; Riehm et al. 2021; Thomeer et al., 2023). To address these gaps, this study aimed to investigate (1) gender and race differences in mental health and psychological well-being among older adults during the pandemic in a nationally representative sample; and (2) whether there are significant interaction effects between gender and race, that is, whether gender differences in mental health and psychological well-being vary by race.
2 Methods
We performed a secondary data analysis utilizing a national dataset. Below, we provide a comprehensive description of our data and sample, as well as the measures and statistical analyses employed in our study.
2.1 Data and Sample
The National Health and Aging Trends Study (NHATS)Footnote 1 is a longitudinal study that annually surveys a nationally representative sample of Medicare beneficiaries ages 65 and older living in the contiguous United States (Freedman et al. 2023). For more detailed information on the NHATS’s sample design, please refer to the NHATS website.1 Our study used the linked NHATS Round 10 and COVID-19 public use data files (Freedman and Hu 2020). The COVID-19 data file is a supplement to the NHATS and collected information about respondents’ experiences during the COVID-19 outbreak from June 2020 to January 2021 in the United States (n = 3257). Our study focused on the mental health and psychological well-being section that includes six dependent variables: loneliness, no time to yourself, poor sleep quality, anxiety, depression, and PTSD. The sample consisted of 2465 respondents after applying three exclusion criteria: (1) not living in a community setting (n = 250, 7.7%); (2) having a proxy respondent (n = 529, 16.2%); and (3) having missing data for the independent or control variables (n = 13, 0.4%). The sample sizes vary among the six dependent variables from 2277 to 2434.
2.2 Measures
Our study incorporated six dependent variables, two independent variables, and a list of control variables in our data analysis.
2.2.1 Dependent Variables
Loneliness
Respondents were asked on a 5-point Likert scale ranging from “never” to “every day,” “During the COVID-19 outbreak, in a typical week, how often have you felt lonely?” Based on their responses, respondents were grouped into two groups: (1) never/rarely and (2) some days/most days/every day.
No Time to Yourself
Respondents were asked on a 5-point Likert scale ranging from “never” to “every day,” “During the COVID-19 outbreak, in a typical week, how often have you felt you couldn’t get any time to yourself?” Based on their responses, respondents were grouped into two groups: (1) never/rarely and (2) some days/most days/every day.
Sleep Quality
Respondents were asked on a 3-point scale ranging from “good” to “poor,” “During the COVID-19 outbreak, in a typical week, how would you rate the quality of your sleep?” Based on their responses, respondents were grouped into two groups: (1) good and (2) fair/poor.
Anxiety
Respondents were asked on a 4-point Likert scale ranging from “not at all” to “severe,” “During the COVID-19 outbreak, in a typical week, how worried or anxious have you felt about the outbreak?” Based on their response, respondents were grouped into two groups: (1) not at all/mild and (2) moderate/severe.
Depression
Respondents were asked on a 4-point Likert scale ranging from “not at all” to “severe,” “During the COVID-19 outbreak, in a typical week, how sad or depressed have you felt about the outbreak?” Based on their response, respondents were grouped into two groups: (1) not at all/mild and (2) moderate/severe.
PTSD
The NHATS survey used PTSD-8 to evaluate respondents’ post-traumatic stress symptoms during the pandemic. The PTSD-8 has eight items with good reliability and validity in different populations including older adults (Hansen et al. 2010). The NHATS adapted six out of the eight-item scale, which includes (1) recurring thoughts about the outbreak and its effects; (2) recurring nightmares about the outbreak and its effects; (3) avoiding activities that remind you of the outbreak and its effects; (4) avoiding thoughts or feelings about the outbreak and its effects; (5) feeling jumpy or easily startled; and (6) feeling on guard. Each symptom was assigned a score of 1 to 4 (1 = none at all, 2 = rarely, 3 = sometimes, 4 = most of the time) based on the frequency of symptoms experienced by respondents. The sum score ranged from 6 to 24, with a higher score indicating higher levels of PTSD symptoms. The Cronbach’s alpha for the 6-item PTSD scale was 0.82 in this study.
2.2.2 Independent Variables
Gender
Respondents were grouped into two categories: males and females. The data did not include gender-fluid participants.
Race and Ethnicity
Race and ethnicity were self-reported by study participants. Respondents were grouped into three categories: Black, non-Hispanic (hereafter, Black); White, non-Hispanic (hereafter, White); and Hispanic or other racial and ethnic group. Participants from Indian, Asian, Native Hawaiian, Pacific Islander, and other races were grouped together with Hispanics because of the small sample sizes.
2.2.3 Control Variables
We controlled sociodemographic and health-related variables, which were potential confounders. Sociodemographic variables included age (65–79 and 80+ years), education level (less than high school, high school or equivalent, and bachelor’s degree or above), location (metropolitan and non-metropolitan), living arrangements (living alone, living with spouse/partner only, and living with others). Health-related variables included self-rated health (poor/fair, good, and very good/excellent) and the total number of chronic conditions including arthritis, stroke, high blood pressure, heart disease, heart attack/myocardial infarction, osteoporosis, diabetes, lung disease, cancer, and dementia/Alzheimer’s disease.
2.3 Statistical Analysis
Descriptive statistics were used to describe the characteristics of the study participants. Regarding our outcomes of mental health and psychological well-being, loneliness, no time to yourself, sleep quality, anxiety, and depression were binary variables, and PTSD was a continuous variable. Chi-square tests were performed to investigate the associations between gender or race and binary outcome variables. A t-test was conducted to investigate the association between gender and PTSD. Analysis of variance (ANOVA) was employed to investigate the association between race and PTSD. Multivariate logistic regression models were used to examine gender and race differences in binary mental health and psychological well-being variables. Multivariate linear regression models were employed to examine gender and race differences in PTSD. To explore whether gender differences in mental health and psychological well-being varied by race, an interaction term between gender and race was included. The interaction between gender and race was not statistically significant for loneliness, no time to yourself, sleep quality, and PTSD, respectively. Thus, we did not report its estimate for the four outcomes.
All multivariate models were adjusted for age, education level, location, living arrangements, self-rated health, and the number of health conditions. Multicollinearity was not an issue in this study because the variance inflation factor (VIF) values of all variables were less than 4 (range: 1.04–3.56). In collinearity diagnostics, the VIF values greater than 10 suggest multicollinearity (Pallant 2020). All estimates were population-weighted and standard errors were adjusted for complex survey design, following the recommendations of the user guide for the NHATS data set (DeMatteis 2021). The survey weights account for differential probabilities of selection and adjust for potential bias related to nonresponse to the survey interviews, to have a nationally representative sample. All statistical analyses were completed in Stata Version 16.1 (Stata Corp, College Station, TX). Statistical significance was accepted at the p < 0.05 (2-sided) level.
3 Results
A total of 2,465 older adults were included in this study and the weighted population sample size was 22,661,866. Table 1 summarizes the unweighted and weighted characteristics of the study respondents. More than half of the older adults were female (56% females, 44% males). Approximately 84% were non-Hispanic White older adults, 6% were non-Hispanic Black older adults, and 10% were other racial and ethnic minorities. Roughly 70% of the older adults were aged between 65 and 79 years old, and 30% were 80 years and older. About 8% of the respondents had an education background lower than high school, more than half of the respondents (54%) had at least a high school degree or equivalent, and 38% with a bachelor’s degree or higher. Nearly 83% of the respondents lived in metropolitan areas and only 17% of them lived in a non-metropolitan area. Approximately 29% of the respondents lived alone, 49% only lived with their spouses or partners, and 23% lived with others. On average, older adults had more than 2 chronic conditions. Nearly half (49%) of older adults self-evaluated their health status as very good or excellent, 36% reported good health, and 15% reported fair or poor health.
As shown in Table 2, overall 43% of older adults in this study experienced poor or fair sleep during the pandemic, 35% reported experiencing loneliness, 30% had anxiety symptoms, 23% felt depressed, and 11% had no time to themselves. The average PTSD score was 11 (range: 6–24), which is relatively low. Moreover, female older adults reported poorer mental health and psychological well-being than males. The gender differences are found in both unadjusted (Table 2) and adjusted (Tables 3 and 4) models. Relative to male older adults, females were more likely to experience loneliness, no time to themselves, poor sleep quality, anxiety symptoms, depressive symptoms, and PTSD, after controlling for sociodemographic and health-related variables.
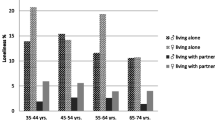
Regarding anxiety and depressive symptoms, there were no significant differences among the three racial and ethnic groups (see Table 2). However, the interaction terms between female and non-Hispanic Black older adults were statistically significant in the multivariate logistic regression models (anxiety symptoms: OR = 0.41, p = 0.010; depressive symptoms: OR = 0.36, p = 0.018; see Table 4). As illustrated in Fig. 1, among non-Hispanic White older adults and other racial and ethnic minorities, female older adults had significantly higher levels of anxiety (Whites: 34% versus 21%; other: 46% versus 22%) and depressive symptoms (Whites: 30% versus 15%; other: 33% versus 16%) than males. In contrast, Black females reported lower levels of anxiety (30% versus 34%) and depressive symptoms (22% versus 24%) than Black males, although the differences were not statistically significant.
Regarding the outcomes of loneliness, sleep quality, no time to yourself, and PTSD, there were no significant interactions between gender and race/ethnicity. As shown in Table 3 and Fig. 2, among the three race/ethnic groups, non-Hispanic Black older adults were the least likely to feel lonely and have poor sleep. There were no significant racial and ethnic differences for no time to yourself. In contrast, as shown in Table 4 and Fig. 3, Black older adults (β = 0.61, p = 0.039) and other race/ethnic minorities (β = 1.23, p = 0.024) were more likely to have PTSD symptoms than non-Hispanic White older adults in the multivariate linear regression model. Although other racial and ethnic minorities were more likely to report PTSD symptoms than Black older adults, the difference was not statistically significant.
Among the control variables (see Tables 3 and 4), we found that older adults with a bachelor’s degree or above were more likely to feel lonely and have anxiety symptoms, depressive symptoms, and PTSD than those receiving high school or less education. Relative to those living with spouses/partners or living with others, older adults living alone were more likely to feel lonely and less likely to have no time to themselves. Older adults living in metropolitan areas were more likely to have poor sleep than those in non-metropolitan areas. Older adults with lower self-rated health reported poorer mental health and psychological well-being, including loneliness, poor sleep, anxiety symptoms, depressive symptoms, and PTSD. Older adults with more chronic conditions reported higher levels of loneliness, poor sleep, and depressive symptoms.
4 Discussion
Using a nationally representative sample of community-dwelling older people aged 65 years or older, this study examined gender, racial and ethnic differences in mental health and psychological well-being during the COVID-19 pandemic. The study found that approximately two out of five older people (43%) experienced poor sleep, followed by loneliness (35%), anxiety (30%), and depression (23%). Overall, females reported poorer mental health and psychological well-being than males, except that Black females had lower but not significant levels of anxiety and depressive symptoms than Black males. Moreover, Black older adults were the least likely to feel lonely and have poor sleep, while White older adults were the least likely to report PTSD and no time to themselves. Our findings strongly support that future policies and interventions should take into account gender and race differences as important considerations to combat pandemic-related stress experiences among older adults with respect to their mental health and psychological well-being.
Consistent with previous studies (González-Sanguino et al. 2020; Gamsızkan et al. 2021; Goveas et al. 2022; Zaninotto et al. 2022), our findings indicate that older females were more vulnerable during the pandemic than males and experienced poor mental health. In general, the proportions of older females reporting depression, loneliness, no time to themselves, anxiety, and poor sleep quality, were 1.91, 1.72, 1.70, 1.51, and 1.24 times the proportions of older males, respectively. Our findings also bring attention to Eagly’s (1987) social role theory, which highlights the link between social behaviors and gender roles. As discussed in the theory, females are expected to act more in the interest of the family and assume caregiving roles (Eagly 1987; Resnick et al. 2022). Women often carry a dual burden of care, managing both housework and working outside to support the family financially (CDC 2019; Sarrasanti et al. 2020). Relative to those in other high-income countries, older adults in the United States were the most likely to report not receiving help during the pandemic such as meal preparation, housework, shopping, or medication management, either from informal caregivers like family or friends or from professional caregivers (Williams et al. 2021). As a result, older females may have to take more care responsibilities. It is significant to note that more than half (53.8%) of women caregivers who are 65 years or older themselves have chronic illnesses and also care for their spouse or close relatives with multiple chronic illnesses and hence experience huge caregiving burden, burnout, and fatigue (CDC 2019). Most commonly these women prioritize the care of their care recipients over their self-care and well-being (Sarrasanti et al. 2020). In line with disaster risk perception and behavioral patterns, women perceived the pandemic as a more serious condition and showed increased compliance towards protective measures against COVID-19 for the safety and well-being of their families (Bruine de Bruin and Bennett 2020; Galasso et al. 2020; Zhao et al. 2020; Gamsızkan et al. 2021). The increased burden of caregiving that women bear further reduces their ability to take rest and secure time for their self-care and well-being and causes increased anxiety, lack of sleep, and suffering (Sarrasanti et al. 2020). Building on prior work, our findings contribute to the new knowledge around the prevalence of poor mental health and psychological well-being during the earlier phase of the pandemic and related disadvantages experienced by older women. Further studies are needed to see the spillover effects of the pandemic on older women’s mental health and well-being among different ethnic and racial groups. Studies suggested that individuals and families were still suffering from post-COVID syndrome that includes prolonged grief, anxiety, and mental health issues (CDC 2022). Awareness and interventions are needed to be in place to screen and provide support to these people to promote their health and well-being in the post-pandemic times.
Our findings reveal a significant interaction between gender and race in relation to anxiety and depression and found within-gender differences among Black older adults. Despite the existing mental health disparities among women at large, Black females reported lower levels of anxiety and depressive symptoms as compared to Black males. Moreover, among all females, Black females had the lowest levels of anxiety, depression, loneliness, and the highest quality of sleep. Similar findings have been reported in other studies during the pandemic (Riehm et al. 2021; Goveas et al. 2022). Black females tend to have a lower risk of anxiety and are found to be resilient despite a higher risk of adversities (Heath 2006; Keyes 2009). Several contributing factors include higher social support and strong cultural and family values that promote their coping abilities during difficult times (Heath 2006; Dale and Safren 2018). The strong Black woman (SBW) schema is a cultural ideal portraying Black women as strong, resilient, self-reliant, nurturing, and self-sacrificing to cope with the stress of gender- and race-based discrimination in their daily lives (Baker et al. 2015). There is a possibility that when Black women were presented with COVID-19, previous lived experiences may have served as a positive coping resource to lessen the negative impacts of the pandemic and achieve better well-being outcomes. However, this SBW schema encapsulates the expectation that Black women must uphold feminine standards as women while also dealing with the added burden of being emotionally and physically strong as Black individuals, a concept known as intersectionality (Collins 2015). Some aspects of the schema seem to be detrimental to health, such as suppressing emotions, resisting feelings of dependence and vulnerability, having an intense motivation to succeed despite limited resources, and feeling an obligation to help others and present an image of strength (Woods-Giscombe et al. 2016). Moreover, when a stressful event persists over a period, the effective coping resources become depleted and the biological systems to buffer the impacts of acute stress may deteriorate health outcomes (Jackson et al. 2010; Gruenewald and Seeman 2010; Baker et al. 2015). This is particularly relevant among older Black women. Although they reported relatively better mental health and psychological well-being during the earlier phase of the pandemic, strategies are warranted to address the deleterious physical and psychological health effects of the chronic stress associated with racial discrimination and other related stressors with aging.
This study also reported that Black older adults were more likely to experience PTSD but less likely to feel lonely and have poor sleep than their White counterparts. There are several possible explanations for our findings. In contrast to White older adults, Black older adults (Whites: 14% and Blacks: 32%) were far more likely to experience economic difficulties during the pandemic (Williams et al. 2021). Black older adults were also more likely to live in multigenerational households and households containing essential workers who were unable to work from home (Macias Gil et al. 2020; Selden and Berdahl 2020). Previous study has found that White individuals are more likely than other minority groups to seek mental health treatment after trauma (Thomeer et al. 2023). Common barriers to not seeking mental health services among Black older adults include fear of stigma, lack of mental healthcare access, and mistrust of healthcare providers (Thomeer et al. 2023). Moreover, being frail and Black creates a double jeopardy of putting off care during the pandemic (Xu and Arling 2023). Frail Black older people were more likely to put off care than frail White older people (Whites: 42% and Blacks: 51%). Similarly, Thomeer et al. (2023) reported that White respondents were most likely to receive professional mental health care before and during the pandemic as compared to Black adults who demonstrated higher levels of unmet mental health care needs during the pandemic. In addition, evidence shows that among Black individuals, faith and spiritual values play a strong role in providing meaning, peace, and comfort during adverse life situations. The coping strategies of religion and positive framing, cultural values, and strong family ties and connections may help explain the low likelihood of loneliness and better sleep among Black older adults (Willey et al. 2022). DeSouza et al. (2021), however, reported that the physical closure of Black churches during the pandemic has caused increased mental stress, particularly among older African Americans. Future studies are therefore needed to examine racial and ethnic differences considering the cultural, religious, and spiritual impacts on older adults’ mental health and well-being.
This study has limitations. First, the COVID sample may be unrepresentative of the older non-White population. Because of the small sample sizes, we have to put Hispanic, Asian, American Indian, or other racial or ethnic groups into one racial and ethnic category. Older adults in this minority category may experience different levels of mental health issues during the pandemic. Future data collection efforts may consider further oversampling racial and ethnic minorities. Second, there are no survey questions pertaining to mental health care-seeking and social support during the pandemic. More information would be beneficial for further investigating the gender and racial differences in mental health and psychological well-being.
5 Conclusion
This study demonstrated a high prevalence of poor mental health and well-being outcomes among older adults during the pandemic. Mental health and psychological well-being vary by gender and race. In general, females reported poorer mental health and psychological well-being than males, except for Black females. Black females had the lowest levels of anxiety, depression, and loneliness, and the highest quality of sleep among all females. We also found that Black older adults were more likely to experience PTSD but less likely to feel lonely and have poor sleep than their White counterparts. Mental health policies and services should be developed and tailored as per the needs of the diverse older adult population rather than adopting a “one size fits all” strategy. Academic-community partnerships can further enhance the understanding of the gaps in mental health services between different genders and races among older adults to enhance their coping, health, and well-being. There is also a need to examine the spillover effects of the pandemic on older adults’ mental health. Lessons learned from the pandemic can guide us in designing and developing future disaster resiliency and recovery frameworks for improving the well-being of older populations.
Notes
Data availability: The National Health and Aging Trends Study (NHATS) Public Use Data files are available at https://www.nhats.org/.
References
Alobuia, W.M., N.P. Dalva-Baird, J.D. Forrester, E. Bendavid, J. Bhattacharya, and E. Kebebew. 2020. Racial disparities in knowledge, attitudes and practices related to COVID-19 in the USA. Journal of Public Health 42(3): 470–478.
Azar, K.M.J., Z.J. Shen, R.J. Romanelli, S.H. Lockhart, K. Smits, S. Robinson, S. Brown, and A.R. Pressman. 2020. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Affairs 39(7): 1253–1262.
Baker, T.A., N.T. Buchanan, C.A. Mingo, R. Roker, and C.S. Brown. 2015. Reconceptualizing successful aging among black women and the relevance of the strong black woman archetype. Gerontologist 55(1): 51–57.
Boserup, B., M. McKenney, and A. Elkbuli. 2020. Disproportionate impact of COVID-19 pandemic on racial and ethnic minorities. The American Surgeon 86(12): 1615–1622.
Bruine de Bruin, W., and D. Bennett. 2020. Relationships between initial COVID-19 risk perceptions and protective health behaviors: A national survey. American Journal of Preventive Medicine 59(2): 157–167.
Carr, D. 2021. COVID-19: Trends, disparities, and consequences for older adults. The Journals of Gerontology: Series B 76(3): e65–e67.
CDC (Center for Disease Control and Prevention). 2019. Caregiving for family and friends—A public health issue. https://www.cdc.gov/aging/caregiving/caregiver-brief.html. Accessed 26 May2023.
CDC (Center for Disease Control and Prevention). 2022. Long COVID or post-COVID conditions. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html. Accessed 26 May 2023.
Collins, P.H. 2015. Intersectionality’s definitional dilemmas. Annual Review of Sociology 41: 1–20.
Dale, S.K., and S.A. Safren. 2018. Resilience takes a village: Black women utilize support from their community to foster resilience against multiple adversities. AIDS Care 30(Supplement 5): S18–S26.
DeMatteis, J.M., V.A. Freedman, R. Jiao, and J.D. Kasper. 2021. National health and aging trends study development of round 10 survey weights. NHATS technical paper #28. Baltimore, MD: Johns Hopkins University School of Public Health.
DeSouza, F., C.B. Parker, E.V. Spearman-McCarthy, G.N. Duncan, and R.M.M. Black. 2021. Coping with racism: A perspective of COVID-19 church closures on the mental health of African Americans. Journal of Racial and Ethnic Health Disparities 8(1): 7–11.
Eagly, A.H. 1987. Sex differences in social behavior: A social-role interpretation. New York: Psychology Press.
Ferrín, M. 2022. Reassessing gender differences in COVID-19 risk perception and behavior. Social Science Quarterly 103(1): 31–41.
Freedman, V.A., and M. Hu. 2020. COVID-19 supplement to the national health and aging trends study user guide. Beta release. v. 3. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health.
Freedman, V.A., J.A. Schrack, and M.E. Skehan. 2023. National health and aging trends study user guide: Rounds 1–12 beta release. Baltimore: Johns Hopkins Bloomberg School of Public Health.
Galasso, V., V. Pons, P. Profeta, M. Becher, S. Brouard, and M. Foucault. 2020. Gender differences in COVID-19 attitudes and behavior: Panel evidence from eight countries. Proceedings of the National Academy of Sciences of the United States of America 117(44): 27285–27291.
Gamsızkan, Z., M. Ali Sungur, and G. Erdemir. 2021. How do older age, gender and risk groups affect protective behaviours and mental health in the COVID-19 pandemic? International Journal of Clinical Practice 75(6): Article e14150.
Garcia, M.A., P.A. Homan, C. García, and T.H. Brown. 2021. The color of COVID-19: Structural racism and the disproportionate impact of the pandemic on older black and Latinx adults. The Journals of Gerontology: Series B 76(3): e75–e80.
García-Fernández, L., V. Romero-Ferreiro, S. Padilla, P.D. López-Roldán, M. Monzó-García, and R. Rodriguez-Jimenez. 2021. Gender differences in emotional response to the COVID-19 outbreak in Spain. Brain and Behavior 11(1): Article e01934.
Goldmann, E., D. Hagen, E.E. Khoury, M. Owens, S. Misra, and J. Thrul. 2021. An examination of racial and ethnic disparities in mental health during the COVID-19 pandemic in the U.S. South. Journal of Affective Disorders 295: 471–478.
González-Sanguino, C., B. Ausín, M.Á. Castellanos, J. Saiz, A. López-Gómez, C. Ugidos, and M. Muñoz. 2020. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain, Behavior, and Immunity 87: 172–176.
Goveas, J.S., R.M. Ray, N.F. Woods, J.E. Manson, C.H. Kroenke, Y.L. Michael, A.H. Shadyab, and J.R. Meliker et al. 2022. Associations between changes in loneliness and social connections, and mental health during the COVID-19 pandemic: The women’s health initiative. The Journals of Gerontology: Series A 77(Supplement_1): S31–S41.
Gruenewald, T.L., and T.E. Seeman. 2010. Stress and aging: A biological double jeopardy?. Annual Review of Gerontology and Geriatrics 30: 155–177.
Hansen, M., T.E. Andersen, C. Armour, A. Elklit, S. Palic, and T. Mackrill. 2010. PTSD-8: A short PTSD inventory. Clinical Practice and Epidemiology in Mental Health 6: 101–108.
Heath, C.D. 2006. A womanist approach to understanding and assessing the relationship between spirituality and mental health. Mental Health, Religion & Culture 9(2): 155–170.
Jackson, J.S., K.M. Knight, and J.A. Rafferty. 2010. Race and unhealthy behaviors: Chronic stress, the HPA axis, and physical and mental health disparities over the life course. American Journal of Public Health 100(5): 933–939.
Jin, J.M., P. Bai, W. He, F. Wu, X.F. Liu, D.M. Han, S. Liu, and J.K. Yang. 2020. Gender differences in patients with COVID-19: Focus on severity and mortality. Front Public Health 8: Article 152.
Keyes, C.L.M. 2009. The Black-White paradox in health: Flourishing in the face of social inequality and discrimination. Journal of Personality 77(6): 1677–1706.
Lalani, N., D.J. Xu, C. Yun, and G.W. Arling. 2023. Structural equation model of coping and life satisfaction of community-dwelling older people during the COVID-19 pandemic. Journal of Patient-Reported Outcomes 7(1): Article 46.
Laufer, A., and M. Shechory Bitton. 2021. Gender differences in the reaction to COVID-19. Women Health 61(8): 800–810.
Macias Gil, R.M., J.R. Marcelin, B. Zuniga-Blanco, C. Marquez, T. Mathew, and D.A. Piggott. 2020. COVID-19 pandemic: Disparate health impact on the Hispanic/Latinx population in the United States. The Journal of Infectious Diseases 222(10): 1592–1595.
Muñoz-Price, L.S., A.B. Nattinger, F. Rivera, R. Hanson, C.G. Gmehlin, A. Perez, S. Singh, B.W. Buchan, et al. 2020. Racial disparities in incidence and outcomes among patients with COVID-19. JAMA Network Open 3(9): Article e2021892.
Pallant, J. 2020. SPSS survival manual: A step by step guide to data analysis using IBM SPSS. New York: Routledge.
Price-Haywood, E.G., J. Burton, D. Fort, and L. Seoane. 2020. Hospitalization and mortality among black patients and white patients with COVID-19. New England Journal of Medicine 382(26): 2534–2543.
Resnick, B., E. Galik, R. McPherson, M. Boltz, K. Van Haitsma, and A. Kolanowski. 2022. Gender differences in disease, function, and behavioral symptoms in residents with dementia. Western Journal of Nursing Research 44(9): 812–821.
Riehm, K.E., S.G. Brenneke, L.B. Adams, D. Gilan, K. Lieb, A.M. Kunzler, E.J. Smail, and C. Holingue et al. 2021. Association between psychological resilience and changes in mental distress during the COVID-19 pandemic. Journal of Affective Disorders 282: 381–385.
Sarrasanti, N., F.K. Donkor, C. Santos, M. Tsagkari, and C. Wannous. 2020. Its about time we care about an equitable world: Women’s unpaid care work and COVID-19. IEEE Engineering Management Review 48(4): 37–45.
Selden, T.M., and T.A. Berdahl. 2020. COVID-19 and racial/ethnic disparities in health risk, employment, and household composition. Health Affairs 39(9): 1624–1632.
Thomeer, M.B., M.D. Moody, and J. Yahirun. 2023. Racial and ethnic disparities in mental health and mental health care during the COVID-19 pandemic. Journal of Racial and Ethnic Health Disparities 10(2): 961–976.
Webb, L.M., and C.Y. Chen. 2022. The COVID-19 pandemic’s impact on older adults’ mental health: Contributing factors, coping strategies, and opportunities for improvement. International Journal of Geriatric Psychiatry. https://doi.org/10.1002/gps.5647.
Willey, B., K. Mimmack, G. Gagliardi, M.L. Dossett, S. Wang, O.J. Udeogu, N.J. Donovan, J.R. Gatchel, et al. 2022. Racial and socioeconomic status differences in stress, posttraumatic growth, and mental health in an older adult cohort during the COVID-19 pandemic. eClinicalMedicine 45: Article 101343.
Williams II, R.D., A. Shah, M.M. Dot, K. Fields, and M. FitzGerald. 2021. The impact of COVID-19 on older adults: Findings from the 2021 international health policy survey of older adults. https://www.commonwealthfund.org/publications/surveys/2021/sep/impact-covid-19-older-adults. Accessed 26 May 2023.
Woods-Giscombe, C., M.N. Robinson, D. Carthon, S. Devane-Johnson, and G. Corbie-Smith. 2016. Superwoman schema, stigma, spirituality, and culturally sensitive providers: Factors influencing African American women’s use of mental health services. Journal of Best Practices in Health Professions Diversity 9(1): 1124–1144.
Xu, D.J., and G. Arling. 2023. Are frail older people from racial/ethnic minorities at double jeopardy of putting off healthcare during the pandemic? International Journal of Environmental Research and Public Health 20(2): Article 1034.
Ya’qoub, L., I.Y. Elgendy, and C.J. Pepine. 2021. Sex and gender differences in COVID-19: More to be learned! American Heart Journal Plus: Cardiology Research and Practice 3: Article 100011.
Zaninotto, P., E. Iob, P. Demakakos, and A. Steptoe. 2022. Immediate and longer-term changes in the mental health and well-being of older adults in England during the COVID-19 pandemic. JAMA Psychiatry 79(2): 151–159.
Zhao, S.Z., J.Y.H. Wong, Y. Wu, E.P.H. Choi, M.P. Wang, and T.H. Lam. 2020. Social distancing compliance under COVID-19 pandemic and mental health impacts: A population-based study. International Journal of Environmental Research and Public Health 17(18): Article 6692.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xu, D., Lalani, N. & Wang, Y. Gender and Race Differences in Mental Health and Well-Being Among Older Americans During the COVID-19 Pandemic. Int J Disaster Risk Sci (2024). https://doi.org/10.1007/s13753-024-00551-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s13753-024-00551-z